Lipid disorders (dyslipidemia) refer to abnormal levels of cholesterol and/or fats in the blood. Lipids are an energy source that constantly circulate from gut to liver and muscle. Fat and carbohydrates provide the most important form of fuel for exercise and sport activities. During exercise, there are four major endogenous sources of energy: plasma glucose derived from liver glycogenolysis, free fatty acids (FFAs) released from adipose tissue lipolysis and from the hydrolysis of triacylglycerol (TG) in very low-density lipoproteins (VLDL-TG), and muscle glycogen and intramyocellular triacylglycerols (IMTGs) available within the skeletal muscle fibers.
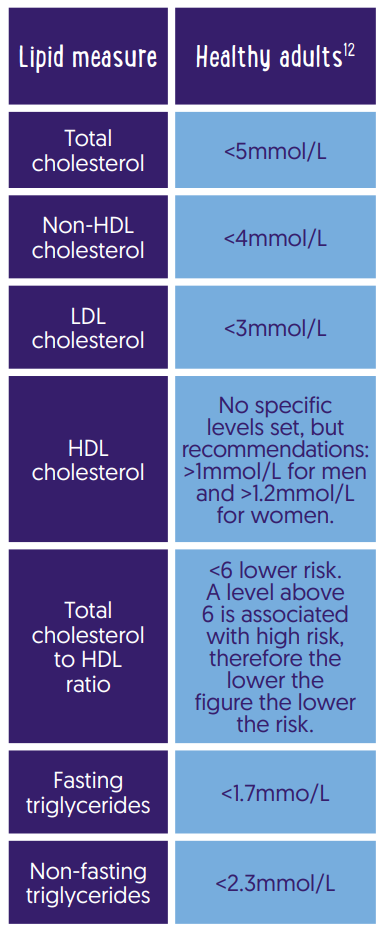
In the past it was easy. High cholesterol meant high risk of heart disease and ultimately high mortality. However, it turns out to be more complicated than that. At the very least, total cholesterol is not very accurate because it is a component of “good” fats (HDL) and “bad” fats (VLDL, IDL, LDL). Having high cholesterol generally refers to having high LDL-C levels, but you can have high Triglycerides or high non-HDL. High-density lipoproteins (HDL) are responsible for carrying cholesterol out of the bloodstream and into the liver, where it is either reused or removed from the body with bile.
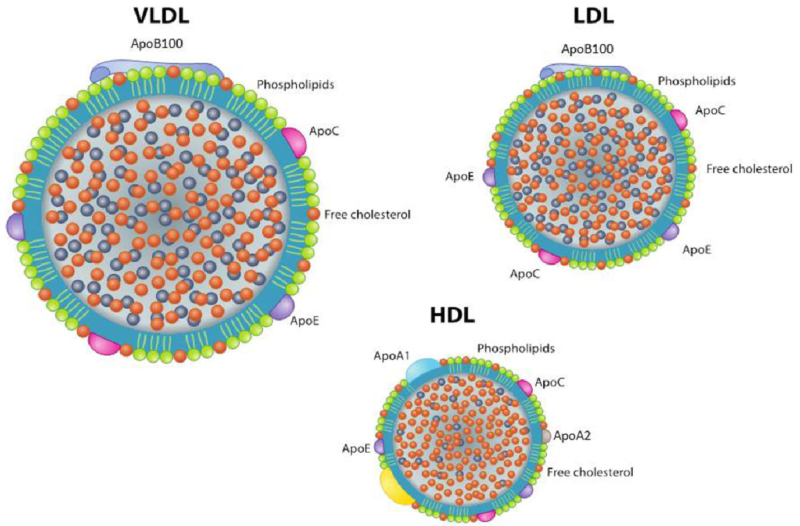
Blood lipoproteins are formed by various amounts of cholesterol (C), triglycerides (TGs), phospholipids, and apolipoproteins (Apos). ApoA1 is the major structural protein of high-density lipoprotein (HDL), accounting for ~70% of HDL protein, and mediates many of the antiatherogenic functions of HDL. Conversely, ApoB is the predominant low-density lipoprotein (LDL) Apo and is an indicator of circulating LDL, associated with higher coronary heart disease (CHD) risk. Thus, the ratio of ApoB to ApoA1 may be a better marker than LDL/HDL itself.

Lipid Pathways
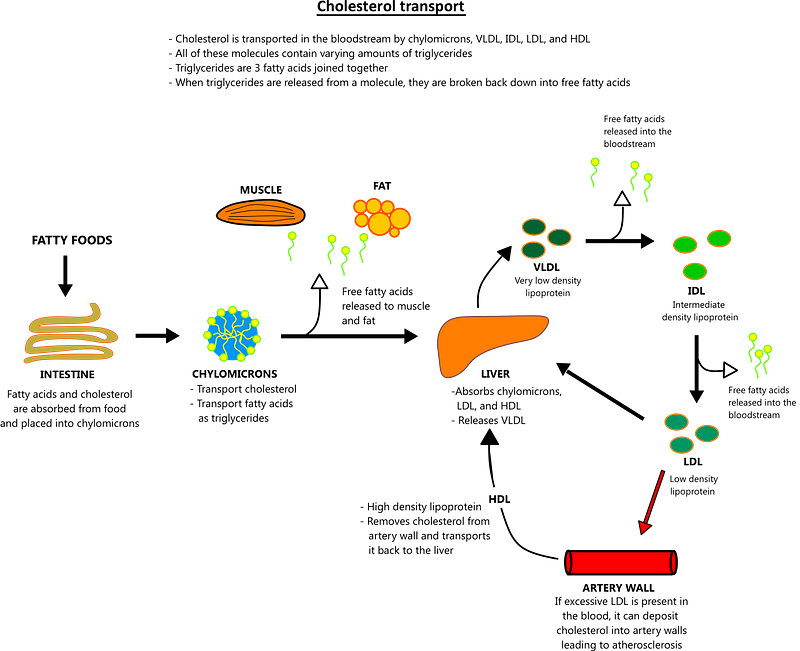
Long-chain FA are absorbed in duodenum and transformed into TGs, that, together with cholesterol and proteins, are assembled as chylomicrons for blood transport. Short- and medium-chain FA diffuse into the blood and are transported to the liver through the hepatic portal vein bound to albumin. TG and cholesterol are transported by four main classes of lipoproteins: very low-density lipoproteins (VLDLs) rich in TG, chylomicrons, low-density lipoproteins (LDLs) rich in cholesterol , and high-density lipoproteins (HDLs). Chylomicrons also deliver dietary cholesterol to the liver, whereas VLDLs are LDL precursors derived from their catabolism. HDLs are essential in plasma lipid transport, providing to the metabolism of chylomicrons and VLDL and removing the excess of unesterified cholesterol from these lipoproteins.
HDLs are involved in a process known as “reverse cholesterol transport,” taking care of the cholesterol transport from peripheral cells to the liver to favor its excretion. HDLs remove cholesterol and fats from cells but also from atheroma of the arterial wall, allowing liver excretion or reutilization. HDL blood concentrations above 60 mg/dL seem to have a protective effect against atherosclerosis
Lipid Abnormalities in Athletes
Even athletes can have high cholesterol, sometimes functional, sometimes dysfunctional. Regular aerobic exercise consistently increases HDL-C, specifically the larger HDL2-C fraction, with more robust effects observed with higher levels of training.Aerobic exercise also decreases LDL-C, smaller LDL particles and triglycerides, but the effects are variable and are more consistent with higher volumes of exercise.Ultra-endurance athletes who have a very low-carbohydrate/high-fat diet may have high LDL-C and HDL-C due to a functional expansion of the circulating cholesterol pool to meet the heightened demand for lipid transport during exercise. Also, a footnote, but recent data points to *very high* levels of HDL-C as potentially deleterious to cardio-vascular health, showing a distinct U-shape association between HDL-C above 100 mg.dL−1 and disease risk.
So most people need to keep your eye on your non-HDL cholesterol or LDL-cholesterol but athletes on low-carbohydrate/high-fat diets may have to watch their HDL specifically.
Lipids and Cardiovascular disease
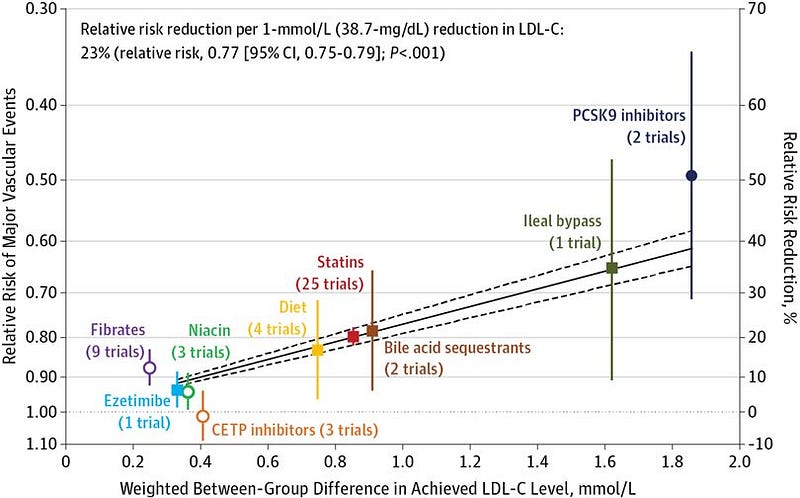
Lipid disorders increase the risk of plaque buildup inside blood vessels, called atherosclerosis or, more generally, cardiovascular disease (CVD). When atherosclerosis occurs in the blood vessels of the heart or brain, it can lead to heart attacks and strokes. Lowering non-HDL cholesterol with both lifestyle changes and medications has been shown to lower the risk of both developing and dying of CVD as shown in this big Lancet study (link).
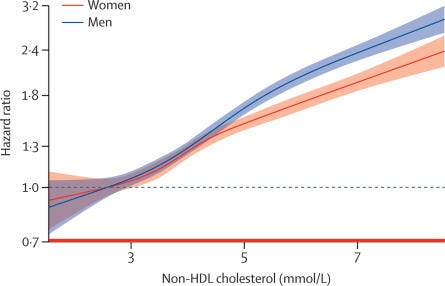
In fact you can use this simple graphic to grade your risk…..

How to check your lipid levels
Here are the approximate healthy lipid ranges…..
in addition, some labs will measure apolipoproteins—ApoA1 and ApoB. They hold the particles inside LDL and HDL together. While ApoA1 holds the “good” HDL, ApoB holds the “bad” LDL particles. So, looking at the ApoB to ApoA1 ratio gives a measure of the “good” versus “bad” cholesterol balance in your blood.
What Contributes to High Cholesterol Levels?
- Age: As people age, their bodies tend to produce more cholesterol [NON-REVERSIBLE]
- Genes: A family history of high cholesterol or heart disease increases a person’s risk of developing high cholesterol [NON-REVERSIBLE]
- Smoking: Nicotine use lowers good cholesterol [REVERSIBLE]
- Being overweight: Excess weight makes the heart work harder in order to pump blood throughout the body, increasing risk of high blood pressure and heart disease [REVERSIBLE]
- Eating a poor diet: People whose diets are high in fat and sugar and low in fruits and vegetables are more likely to develop high cholesterol [REVERSIBLE]
- Living a sedentary life: A lack of exercise increases a person’s risk of high cholesterol [REVERSIBLE]
Diet as a Treatment for Dyslipidaemia
Fortunately, you can reverse your lipid issues provided you make a consistent change in lifestyle. That means reversing all of the reversible risk factors above.
If you want to know what diet to follow, your can either eat a healthy macro diet (eg portfolio diet) or break it down item by item.
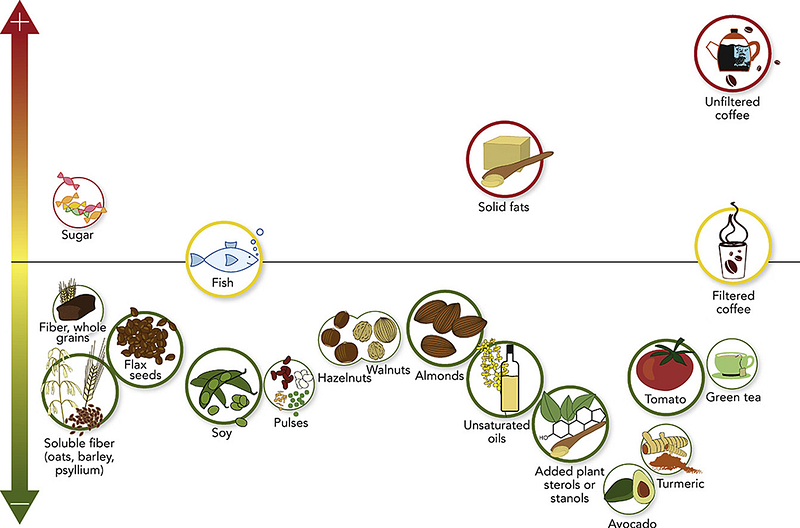
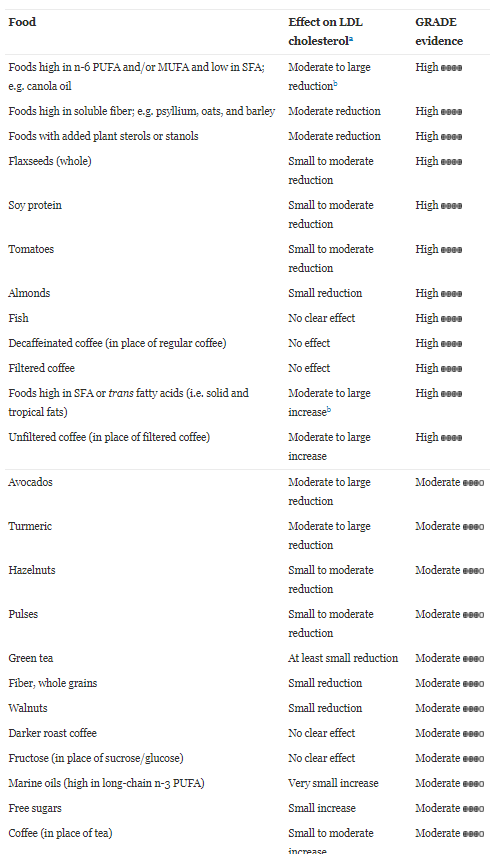
Here is an evidence based review of which foods appear to lower LDL cholesterol in the blood (link)
and if you follow a healthy portfolio diet, these are typical changes…..(see link)
non HDL-C (-14%)
LDL-C (-17%)
TC (-12%)
Apolipprotein B (-15%)
CRP (-32%)
Exercise as a Treatment for Dyslipidaemia
Exercise often improves lipid profile especially in unfit sedentary people. The mechanism might involve adiponectin. Furthermore, after an aerobic exercise there is an increase of ApoA1 and a decrease in ApoB (ApoB/ApoA1 may be a better risk predictor of CHD than LDL/HDL)
Meta-analyses suggest that training period correlate with improvement in lipid profile (ref). Each 10-minute increase in exercise duration corresponded to an increase of 1.4 mg/dL in HDL level.
Regular aerobic training resulted in changes in the levels of
HDL-C (0.4 mg/dL),
LDL-C (-0.18 mg/dL)
TC (- 0.33 mg/dL)
TG (- 0.33 mg/dL)
Resistance training produced changes in the levels of
HDL-C (0.84 mg/dL)
LDL-C (- 0.23 mg/dL)
TC (-0.32 mg/dL)
TG (-1.3 mg/dL)
Drug Treatment for Dyslipidaemia
What if diet fails? Drug treatment with a statin is an option, and provided the drug reduces LDL or non-HDL lipids then there is generally a benefit (figure). But there may be some drug-related risk, hence lifestyle change is preferred IMHO (see link)
Citations
Creighton BC, Hyde PN, Maresh CM, et al Paradox of hypercholesterolaemia in highly trained, keto-adapted athletes BMJ Open Sport & Exercise Medicine 2018;4:e000429. doi: 10.1136/bmjsem-2018–000429
