I was asked recently by a coached rider “should i reduce the amount of high intensity intervals at zone5,z6,z7 due to the possibility of immunosuppression, after all we are all meant to be cautious about coronovirus?”
This is a very reasonable question with two sides: should you go out riding and can you safely go out riding?

Derbyshire police have been spying on people with drones who are out walking and Iron Man triathlete Joe Skipper thinks its fine to ride all day because despite UK restrictions, he went out for a 9hr, 325 km bike ride. Despite lots of hysteria about this, I doubt he was posing a risk to anyone including himself. 41% of accidents are in the home, only 25% during leisure and 15% on the road, so you could argue it wasn’t even a question of resources if he had a problem. BUT he probably should have followed national rules which are to stay at home or local where possible. Alternatively he could have said he was a pro and needed special permission to train long before doing it. Now everyone hates him for doing what was entirely normal a month ago and he has had to delete his strava account.

Many people are scared about the health effects of over-exercising, and the effects on the immune system. My first instinct is to say I don’t think there is any problem; after all there is not a whole hospital ward of athletes in hospital following the each olympics because of stress-related infections. However these are anxious times. Italy, Spain and France have banned all recreational cycling outdoors. In UK, Germany and Belgium governments are encouraging people to use their bikes if they have to get to work but this could change. Group exercise is generally banned, and most events have been cancelled. However in most countries you can ride solo outdoors, and in all countries you can train indoors.
So let’s examine the question of whether intense exercise promotes dysfunctional immune suppression (leading to illness and complications)
INTRODUCTION
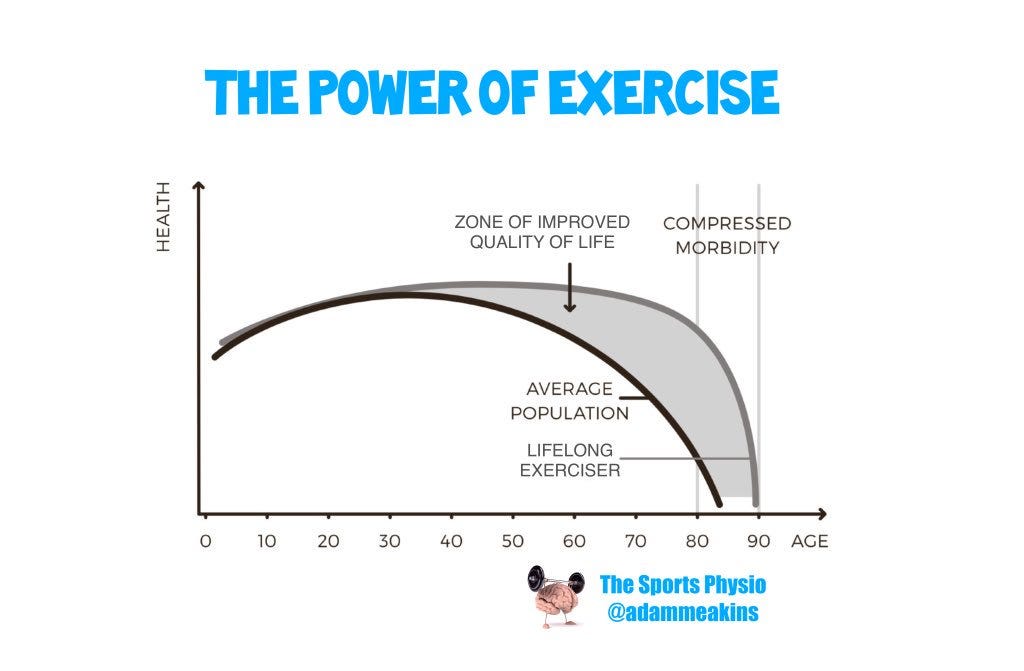
Lifelong physical activity is one of the most healthy things you can do, rivaled only perhaps by giving up smoking and giving up eating deep fried mars bars.

Long term exercise reduces the risk of chronic diseases such as cancer, respiratory disease, and cardiovascular disease. The overall effect on mortality is nothing short of stunning, with a strong dose-response relationship between exercise and reduced mortality. It also improves quality of life dramatically whilst your are living…..it’s a win-win!
Less known is that exercise also reduces chances communicable diseases including viral and bacterial infections.

However does very intense or very long endurance exercise promote infection (even if temporarily)? This would be a J-shaped curve .

This hypothesis infers that those who undertake an “excessive” exercise, over a period of days or weeks and months are not only at risk of “over-training” but may be at a greater risk of infections.
Athletes and Risk of Infections: Early evidence
One of the first studies from this era found that one third of 150 runners participating in the 1982 “Two Oceans” 56 km ultramarathon in Cape Town South Africa self-reported symptoms of upper respiratory tract infections (URTI) with symptoms = runny nose, sore throat, sneezing within 2 weeks of the race (link). The control group, who were age matched and shared a home with another of the race competitors, reported only half the amount of URTIs in the same period. Similar observations were made in 1987 Los Angeles Marathon (link). Of 2,311 respondents who had completed the marathon and whom did not report an infection in the week prior to the race, 12.9% reported an infection in the week after the race compared to only 2.2% of individuals who withdrew from the race for reasons other than illness (odds ratio 5.9).
BUT
More recent prospective cohort study of 1,509 Swedish men and women aged 20–60 years found that higher physical activity levels were associated with a lower incidence of self-reported URTIs (link). Studies of ultramarathon runners, who undertake the largest volume of exercise among athletes, have shown that these individuals report fewer days missed from school or work due to illness compared to the general population. For example, the mean number of sickness days reported over 12 months was 1.5 days in a study of 1,212 ultramarathon runners and 2.8 days in a study of 489 ultramarathon runners (link).
So the situation is unclear, so let’s look at the evidence from good quality studies in more detail….
Normal Exercise and Risk of Infections

Several large studies have examined illness in those undertaking physical exercise. I am talking about normal levels of exercise within your normal capabilities, whatever that is for you. So if you did 4 hours last week, it might be lets say under 6 hours at yes at broadly the same overall intensity. So if your TSS (training stress score) was 100 last week then lets says 80–120 this week……ie a TSB (balance) of no less than -20.
btw you can find my entire video on fitness fatigue and burnout here:
back to the studies….
Mathews et al. (ref101) looked at 547 male and female adults (aged 48.0 ± 12.4 years). There was 29% decreased illness risk in upper vs. lower quartile of activity, meaning those that did more faired better.
Fondell et al. (ref102) looked at 1509 male and female adults (aged 20–60 years). There was an 18% decreased illness risk in high vs. low physical activity.
Nieman et al. (ref 103) looked at 1002 male and female adults (aged 18–85 years). There was a 46% decrease in total day with illness in high vs. low physical fitness tertile. 43% decrease in those who reported ≥5 days/week aerobic activity vs. <1 day/week.

Zhou et al.(ref 104) looked at 1413 male and female adults (aged 38.9 ± 9.0 years). There was an 26% decreased illness risk in high vs. low physical activity.
Collectively, these large epidemiologic studies consistently show reduced URTI rates (weighted mean, -28%) in high exercise groups vs. low physical activity and fitness groups. So basically that’s good news: you should keep exercising (or maybe start exercising!). BUT what happens if you do way more than average, eg +25% in volume and intensity in one day or week……
High Volume / Ultra-Events and Risk of Infections

What I have discussed so far, is normal range of exercise (that 98% of the population who exercise do) but what happens if you do ultra-events, eg marathon, iron-man or longer and are not ready for them? And what happens if you do way too much, like a crazy duracell bunny?
Comparative studies
Five studies compared illness rates, largely URTI in high volume elite athletes vs controls doing mostly normal exercise rates.
Peters and Bateman (ref 67) looked at 141 ultramarathon runners and 124 controls (aged 18–65 years). Illness incidence was higher, 33% vs. 15% after race in runners vs. controls.
Nieman et al (ref 21) looked at 1828 marathon runners and 134 runner controls (aged 36.9). Illness incidence was higher 13% vs. 2% in runners who finished race vs. controls. Interestingly runners training ≥97 km/week were at higher URTl risk.
Rama et al (ref 73) looked at 19 elite swimmers vs. 11 non-athlete controls (aged 17.6 ± 1.0 years). 67% of illness episodes occurred during high volume training in swimmers vs. no illness in control at same time points but this was a small study.
Svendsen et al (ref 75) looked at 42 elite cross-country skiers (aged 24 ± 4 years) vs controls. Illness incidence was 3× higher in skiers who raced the Tour de Ski vs. non-competing skiers (48% vs. 16%).
One study very interesting compared elite vs recreational vs sedentary folks. Spence et al (ref 71) looked at 20 elite triathletes/cyclists, 30 recreational triathletes/cyclists, 20 sedentary controls (aged 18–34 years). Illness incidence was 4× higher in elite athletes and 2× greater in controls compared with recreational athletes. So that one study supports the j-shaped curve hypothesis. In fact there were a higher number of illness days in elite athletes (311 days) and control (137 days) vs recreational (92 days). So to repeat recreational levels in this study were best.
Risk Factors for infection
A handful of studies attempt to look at risk factors because, after all , most elite athletes DO NOT get unwell, and most UrTI symptoms are mild and transitory. Serious infections are very rare indeed as a result of training.
Heath et al.(ref 69) looked at 530 runners (aged 39.4 years). Those who ran >485 miles/year (780 km/year) had an increased risk of illness.
Konig et al. (ref 70) looked at 852 German athletes (aged 23.6 ± 9.5 years). Illness was 2× higher in endurance sports / with stress and with sleep deprivation.
Timpka et al. (ref 80) looked at 3305 elite track and field athletes during the international World Championships. Illness was 10× greater illness incidence in endurance events.
Other illness risk factors include female gender, high levels of depression or anxiety, engaging in unusually intensive training periods with large fluctuations, international travel across several time zones, participation in competitive events especially during the winter, lack of sleep, and poor diet.
OK so there seems to be a slight risk of low grade URTI after intense exercise but is it backed up by physiology? lets briefly look at what is actually going on in the blood and immune system……
Blood Markers after Acute vs Long Term Exercise
Acutely
Upon exercise cessation, there is a biphasic exercise response is characterized by a decrease in lymphocytes (white cells) in the bloodstream and a sharp recovery. The low point (nadir) is typically observed approximately 1–2 h post-exercise when the lymphocyte numerical count is lower than pre-exercise levels BUT lymphocyte frequency normally returns to pre-exercise levels within 24 h. The lymphopenia (low levels) that occurs 1–2 h later is exercise intensity dependent and the most profound reductions during this period are typically observed among natural killer cells and CD8+ T cells. Others have noted decreases in circulating numbers of Type 1 T cells, inhibition of cell cytokine production, reduced T cell proliferative responses and falls in stimulated B cell immunoglobulin synthesis.An indirect marker of this may be reduced salivary IgA.
But the reduction in lymphocytes (and other immune cells) in peripheral blood in the hours following vigorous and prolonged exercise does not reflect immune suppression. Instead it is now thought to be heightened state of immune surveillance and immune regulation driven by a preferential mobilization of cells to peripheral tissues. As such, nutritional interventions, which have been employed to dampen the magnitude of exercise lymphopenia are unlikely to reduce the incidence of infections. Basically immune cells are redistributed out of the bloodstream to tissues and organs where they are needed, just as glucose and hemoglobin are, and this is entirely normal!
Long Term
Long term, training has an overall anti-inflammatory influence mediated through multiple pathways including improved control of inflammatory signaling pathways, release of muscle myokines that stimulate production of IL-1ra and IL-10 (perhaps by blood mononuclear immune cells), a decrease in dysfunctional adipose tissue and improved oxygenation, enhanced innate immune function, and an improved balance of oxylipins.7, 33,50, 55,120
Very Long Term: Aging!
There is strong evidence that regular exercise helps reduce declines in the immune system with age. In other words in the long term multiple immune benefits accrue after regular lifelong exercise…..This is based on:
Lower numbers of exhausted/senescent T cells
Increased T-cell proliferative capacity
Lower circulatory levels of inflammatory cytokines (i.e., decreased “inflamm-aging”),
Increased neutrophil phagocytic activity,
Lowered inflammatory response to bacterial challenge,
Greater NK cell cytotoxic activity, and
Longer leukocyte telomere lengths.
Preventing Exercise Related Stress/Infections
So risk is low, but should you take any precautions? Yes. Helpful tips are:
a. Minimize exposure by avoiding close contact, not sharing drinks or food, avoiding over-crowded areas like gyms
b. Limit hand-to-face contact (i.e., self-inoculation) and wash hands regularly and effectively.
c. Try prioritise rest and sleep and avoid excessive alcohol intake.
d.Consume a well-balanced diet with sufficient energy to maintain a healthy weight.
And regards diet…..
Focus on grains, fruits, and vegetables to provide sufficient carbohydrate and polyphenols .A consistent finding is that carbohydrate intake during prolonged and intense exercise, whether from 6%–8% beverages or sugar-dense fruits such as bananas is associated with reduced stress hormones, diminished blood levels of neutrophils and monocytes, and dampened inflammation. Gut-derived phenolics circulate throughout the body after increased polyphenol intake, exerting a variety of bioactive effects that are important to athletes including anti-inflammatory, antiviral, antioxidative, and immune cell signaling effects.
Carbohydrate ingestion before and during exercise attenuates post-exercise inflammation.

And regarding being cold outside?
Can you catch flu from being outside in the wet and cold? A meta-analysis from Eccles found this was not the case. It’s a myth. Yes in the cold viruses might survive longer and people might gather closely inside
A study done at Wake Forest School of Medicine looked at the distance sneeze and cough particles can travel. It was about 2m/6 feet.
To infect someone, these particles don’t have to be breathed in, they just have to get into any mucosal surface — eyes, mouth or nose. In addition, drops spread by getting on surfaces such as door handles.
Summary & Advice
By exercising you are reducing your likelihood of a vast number of diseases and infections, so the essential message is that exercise is good. There is a short term effect of acute exercise on reduced white cells (and other markers ) in the blood but this is entirely physiological and not a cause of immunosuppression itself!
Large scale studies do show you can exercise too hard for too long and become more prone to (generally mild) symptoms of infection. About half of the acute illness bouts involve the respiratory tract, with other affected systems including the digestive tract, skin tissues, and the genitourinary tract in a small number of cases (ref 65). Severe infections related to exercise are very rare; almost unknown.
Remember that most (in one study 72%) of the population suffer at least 1 non-influenza related URTI over 12 months….so not everything you catch is related to exercise.
So back to my athletes question: “should i reduce the amount of high intensity intervals at zone5,z6,z7 due to the possibility of immunosuppression, after all we are all meant to be cautious about coronovirus?”
Practical Advice
keep exercising, within your normal limits
keep your fatigue level in check (TSB +/- 15)
follow local rules (if only to avoid being arrested)
take extra precautions about carrying equipment for repairs
always take your phone
let someone know where you are and when you are expected back
Citations
